The U.S. Food and Drug Administration (FDA) has issued a Class I recall for Marketside Broccoli Florets (12 oz.) after tests detected potential contamination with Listeria monocytogenes.

A stack of broccoli | Source: Getty Images
Braga Fresh Foods LLC voluntarily initiated the recall on December 27, 2024, affecting 5,918 cases. The recalled packages are labeled “BEST IF USED BY DEC 10 2024” and bear the code BFFG327A6 13:56.
The issue came to light when Texas Health & Human Services conducted random testing at a Walmart store in Texas. Out of multiple samples, one tested positive for Listeria monocytogenes, prompting swift action. So far, no illnesses have been reported in connection with the product, but health officials are urging caution.
According to the FDA, a Class I recall is the most serious category, indicating a “reasonable probability that the use of, or exposure to, a violative product will cause serious adverse health consequences or death.”
Listeria monocytogenes is a bacterium that can cause serious infections, especially in young children, older adults, and people with weakened immune systems. Individuals may experience fever, headache, nausea, stomach pain, and diarrhea, but the infection can be especially dangerous for pregnant women, possibly leading to miscarriages or stillbirths.
Given these health risks, consumers in multiple states may have purchased the affected product. Walmart stores in 20 states received the recalled broccoli florets, including locations in Alaska, Arkansas, Arizona, California, Colorado, Idaho, Illinois, Indiana, Kentucky, Louisiana, Michigan, Montana, Nevada, Ohio, Oklahoma, Oregon, Texas, Utah, Washington, and Wyoming.
Consumers who purchased the recalled product should not consume it and should discard it or return it to the store. Braga Fresh Foods LLC alerted retailers through email, phone, press releases, and direct visits.
The FDA continues to monitor the situation as the recall remains ongoing.
As food safety concerns continue, another recall was issued—this time for organic carrots linked to a separate contamination risk.
On November 17, 2024, the Centers for Disease Control and Prevention (CDC) and the FDA alerted the public to a new E. coli outbreak in the U.S. linked to organic carrots. They revealed which products were recalled, the affected states, case statistics, symptoms, and what people should do to avoid infection.
The CDC and FDA confirmed that the E. coli outbreak was linked to organic whole and baby carrots of multiple sizes distributed by Grimmway Farms.
Although the supplier company issued a recall of the implicated products on November 16, 2024, the CDC warned that some of the recalled bagged carrots could still be in consumers’ homes, even if they were no longer available on store shelves.
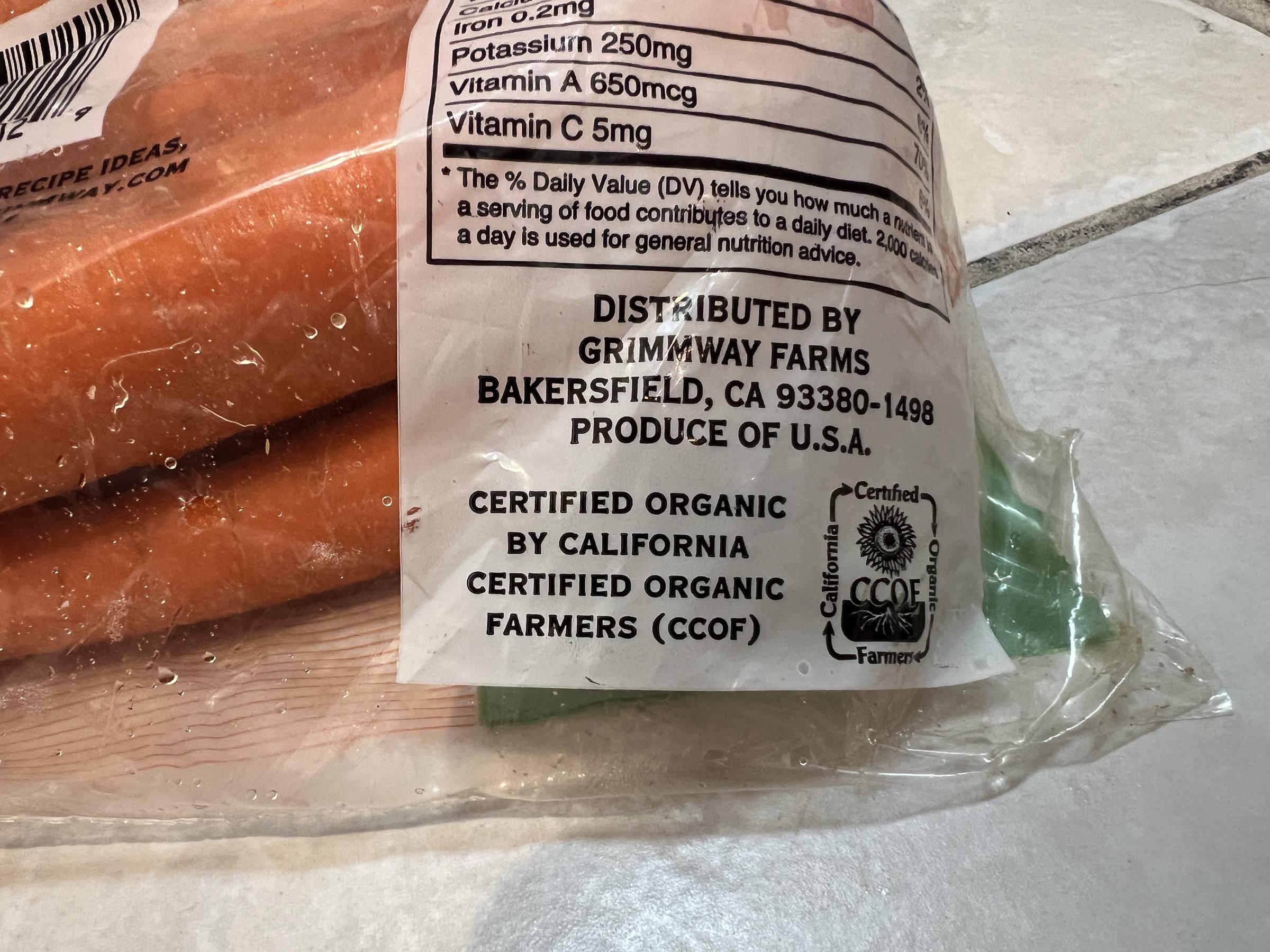
A close-up photo of a Grimmway Farms information label in Lafayette, California on November 17, 2024 | Source: Getty Images
At the time, people were advised to check their refrigerators for any brands of organic whole or baby carrots that had been recalled and to immediately discard or return them to the store.
Businesses were also cautioned against selling such items and were urged to wash and sanitize any surfaces or objects that might have come into contact with the recalled carrots.

An individual holding a bunch of baby carrots from their fridge in Lafayette, California. | Source: Getty Images
Grimmway Farms’ product recall consisted of a comprehensive list of several brands. The affected brands included well-known names such as 365, Bunny Luv, Cal-Organic, Compliments, Full Circle, Good & Gather, GreenWise, and Marketside.

A close-up photo of a packet of Bunny Luv organic carrots from Grimmway Farms in Lafayette, California. | Source: Getty Images
Others included Nature’s Promise, O-Organic, President’s Choice, Raley’s, Simple Truth, Sprouts, Trader Joe’s, Wegmans, and Wholesome Pantry. The recalled baby organic carrots had best-if-used-by dates ranging from September 11 to November 12.
Although the whole organic carrots had no specific best-if-used-by dates listed on the bags, these products were available for purchase in stores between August 14 and October 23. Whole organic carrot brands that were affected by the E. coli product recall were identical to those for the baby carrots.
The E. coli outbreak was confirmed in 18 states across the U.S., with a total of 39 reported illnesses, 15 hospitalizations, and one death. Additionally, the last reported illness onset occurred on October 28.
Affected states included Arkansas, California, Colorado, Massachusetts, Michigan, Minnesota, Missouri, North Carolina, New Jersey, New York, Ohio, Oregon, Pennsylvania, South Carolina, Texas, Virginia, Washington, and Wyoming.
Interviews conducted with 27 individuals who fell ill revealed that 26 (96%) had consumed carrots in the week prior to experiencing symptoms, which solidified the link to the recalled products.
According to a case count map provided by the CDC, states like Minnesota, New York, and Washington were experiencing higher concentrations of cases, with other states such as Wyoming, California, and Texas showing a more scattered spread.
The recalled organic carrots were contaminated with Shiga toxin-producing Escherichia coli (E. coli) O121:H19, which was a dangerous strain of bacteria known to cause severe and sometimes life-threatening infections.
This strain reportedly posed a heightened risk to young children, the elderly, and individuals with compromised immune systems.
In severe cases, E. coli infections can cause complications such as kidney issues, including hemolytic uremic syndrome a.k.a HUS, which may lead to kidney failure or, in extreme cases, death. Common symptoms typically appear three to four days after exposure and include intense stomach cramps, bloody diarrhea, fever, nausea, and vomiting.
Most people recover within five to seven days without treatment, but some develop serious kidney problems that require hospitalization. The CDC urges anyone with severe symptoms, such as dehydration, persistent diarrhea, or a fever over 102°F, to seek medical care immediately.
Escherichia coli, commonly known as E. coli, are bacteria found in food, water, and the intestines of people and animals. While most strains are harmless and support digestion, vitamin production, and immune defense, some can cause severe illness.
Infection often occurs when individuals consume E. coli through contaminated food or water, or direct contact with infected animals, people, or environments.
Vulnerable populations, including adults aged 65 and older and international travelers, are at higher risk of infection.
To minimize the risk of contracting E. coli, the CDC has shared an array of prevention tips that focus on proper food handling, cleanliness, and vigilance with water and beverages.
Frequent handwashing remains one of the most effective ways to reduce the spread of harmful bacteria. Civilians should wash their hands for at least 20 seconds with soap and water before, during, and after food preparation, and always after handling raw ingredients like meat, poultry, or eggs.
Kitchen surfaces, utensils, and cutting boards should also be washed thoroughly with hot, soapy water between uses to prevent cross-contamination. Additionally, fresh fruits and vegetables should be rinsed under running water before consumption.
Keeping raw meat, poultry, seafood, and eggs separate from other foods is also crucial. People should use different cutting boards for raw and ready-to-eat items, and store raw foods in sealed containers to prevent juices from leaking. Notably, the CDC advises against washing raw chicken as it can spread bacteria to kitchen surfaces.
When it comes to cooking food, finding the correct internal temperature is vital for killing harmful bacteria like E. coli. One should also use a food thermometer to ensure accuracy.
The CDC recommends specific temperatures such as 145°F for whole cuts of meat, 160°F for ground meats, and 165°F for poultry and leftovers.
Additionally, people should refrigerate perishable foods promptly (within two hours, or one hour if temperatures exceed 90°F) and keep their refrigerators at 40°F or below to inhibit bacterial growth.
Other prevention measures involve ensuring access to safe drinking water. When camping, hiking, or traveling, people should ensure water is treated to avoid contamination.
Similarly, one should avoid swallowing water while swimming in lakes, ponds, or pools, and never swim if experiencing diarrhea.
Lastly, civilians should only consume milk, juices, and dairy products that are clearly labeled as pasteurized. This process kills harmful germs, including E. coli, and ensures a safer food and beverage experience.
By following these steps, individuals can greatly reduce their risk of E. coli infection and other foodborne illnesses, ensuring the protection of themselves and their loved ones.